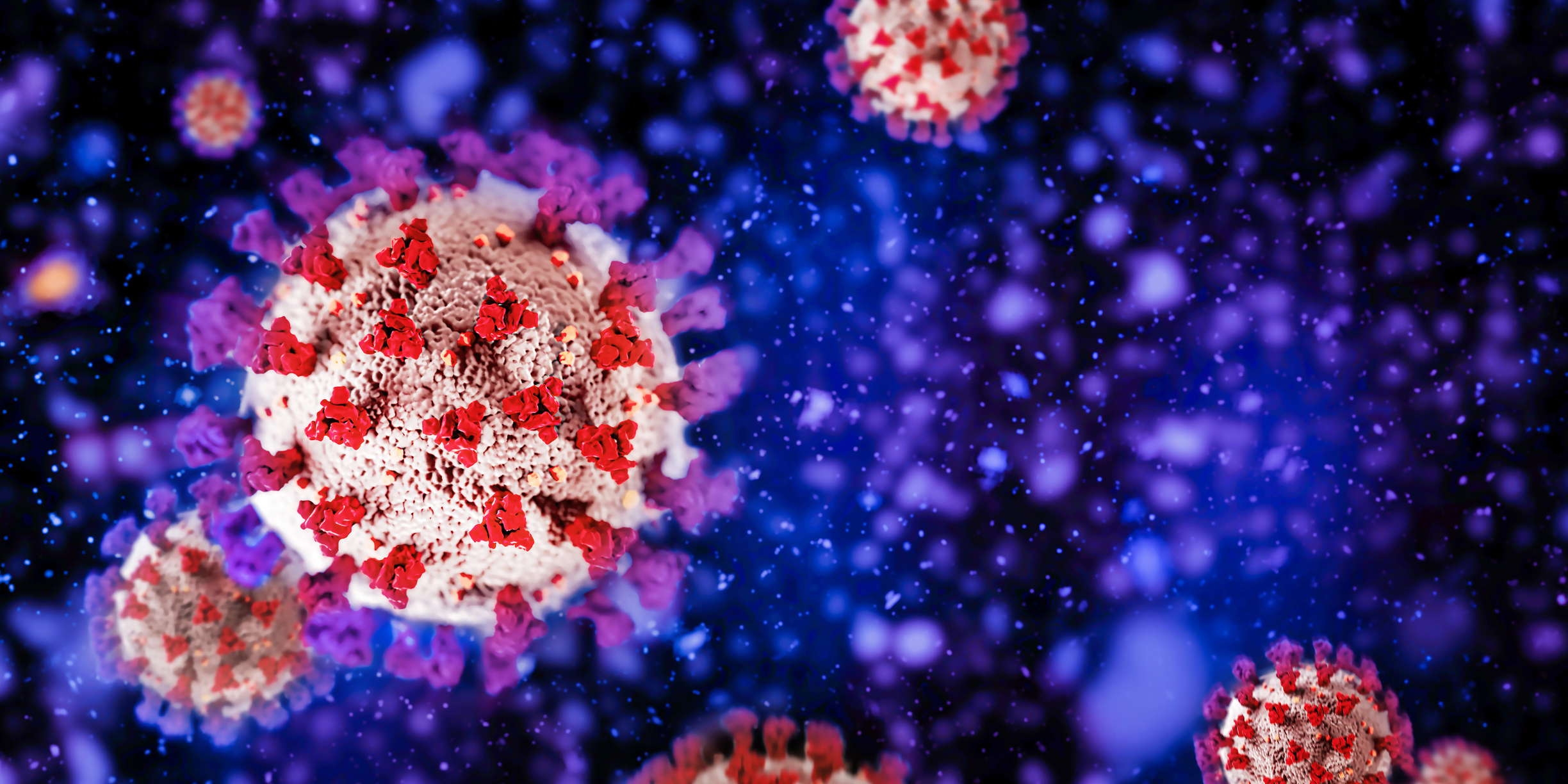
Researchers from the Universities of Arizona, Oxford, and Leeds have conducted a comprehensive review of numerous studies on long COVID, aiming to understand its prevalence, underlying mechanisms, symptoms, and potential treatments.
Long COVID, or post-COVID-19 condition, is characterized by symptoms lasting three months or longer following an acute COVID-19 infection. This illness can affect multiple organ systems, leading to symptoms such as fatigue, cognitive impairment (‘brain fog’), breathing difficulties, and various forms of discomfort.
The study reveals that long COVID can impact individuals of all ages, including children. It is notably more common among females and those from lower socioeconomic backgrounds, though the reasons for these disparities remain under investigation. While some individuals gradually recover, others may experience persistent symptoms for years. Notably, many who contracted long COVID before vaccines became available continue to suffer.
“Long COVID is a devastating disease with a profound human toll and socioeconomic impact,” said Dr. Janko Nikolich, senior author of the study, director of the Aegis Consortium at the University of Arizona Health Sciences, and a professor at the University of Arizona College of Medicine. “By studying it in detail, we hope to understand the mechanisms and identify therapeutic targets, which could also benefit other chronic conditions like myalgic encephalomyelitis/chronic fatigue syndrome and fibromyalgia.”
Vaccination and boosters significantly reduce the risk of long COVID. However, 3%-5% of individuals worldwide still develop the condition after an acute COVID-19 infection. In the U.S., the Centers for Disease Control and Prevention estimate that long COVID affects 4%-10% of the adult population, with 1 in 10 adults who had COVID developing long-term symptoms.
The review highlights various biological mechanisms involved in long COVID, including the persistence of the virus in the body, immune system disruptions, and microscopic blood clotting, even in individuals with mild initial infections.
Currently, there are no proven treatments for long COVID. Management focuses on symptom relief and rehabilitation. Researchers stress the urgent need for biomarkers, such as blood tests, to diagnose and monitor long COVID, and for therapies addressing the root causes of the disease.
Preventative measures include avoiding infection through mask-wearing in crowded indoor spaces, promptly taking antivirals if infected, avoiding strenuous exercise during infection, and staying up-to-date with vaccinations and boosters.
“Long COVID is a dismal condition, but there are grounds for cautious optimism,” said Professor Trisha Greenhalgh, lead author of the study from Oxford’s Nuffield Department of Primary Care Health Sciences. “Mechanism-based treatments are being tested in trials. If effective, these could provide precision therapies for specific subgroups. It is increasingly clear that long COVID imposes a significant social and economic burden. We need better ways to treat and support ‘long-haulers’—those unwell for two years or more, whose lives have been severely impacted.”
This study underscores the urgent need for continued research and development of effective treatments to alleviate the burden of long COVID on individuals and society.
(ANI)